Data Intelligence & Transformation in Physician-Owned Practices

Executive Summary
The U.S. healthcare industry is navigating a fundamental transformation driven by unsustainable costs, an aging population, and a rapid technological revolution. For physician-owned private practices, this environment presents a "trust paradox": while clinicians recognize data as a strategic asset, they are often overwhelmed by the administrative burden of managing it. Reportedly, 65% of data leaders believe employees trust their information, a significant "governance lag" persists, as 76% of companies report that organizational oversight cannot keep pace with rapid AI adoption. These critical vulnerabilities are compounded by documentation-driven burnout with physicians spending over a third of their time on paperwork and fragmented data silos that stifle clinical accountability and care coordination.
However, the convergence of "agentic AI" and "decision intelligence" offers a $1 trillion opportunity to shift industry spending toward digital-first, proactive models that meet the demands of an increasingly empowered "super consumer". This white paper outlines the current pain points, including EHR-driven burnout and data siloing and identifies industry trends such as the integration of "agentic AI" and "decision intelligence". By adopting unified technology solutions and robust data governance, private practices can shift from reactive models to proactive, personalized care, ultimately recapturing clinician time and ensuring financial sustainability in an increasingly competitive market.
1. Introduction
The Landscape of Private Practice (2026 and Beyond)
The current healthcare landscape is defined by a shift in economic leverage and a "super consumer" who demands seamless digital experiences. As of 2026, technology is no longer merely augmenting healthcare; it is becoming the system. While historically many physicians opted for private practice for independence and financial stability, the model is under intense pressure. Larger hospital systems are leaning into tech-based transformations, leaving independent practices to find their own paths to resilience through innovation.
Industry Trends at a Glance:
- The Aging Population: By 2030, there will be more Americans over 65 than under 18, increasing the demand for complex chronic and geriatric care.
- AI Adoption Acceleration: AI adoption is growing faster than any other technology in recent history, specifically in prior authorization, revenue cycle management (RCM), and documentation.
- Value-Based Care Shift: Payers are pressuring providers to take on financial risk, necessitating sophisticated analytics and team-based care models to manage larger risk pools.
- The Rise of Private Capital: Private equity and venture capital investment in physician practices have surged, reaching $60 billion by late 2019 and continuing to accelerate into 2026 to drive practice expansion and infrastructure modernization.
2. Critical Data Management Pain Points
Physician-owned practices face a unique set of obstacles in the data-driven era, primarily stemming from fragmented infrastructure and administrative overload. Physicians spend more than a third of their time over 1.5 days a week on paperwork. This "pajama time" spent on after-hours charting is a leading cause of burnout, with 44% of physicians reporting unresolvable stress.
Key Challenges:
- EHR Usability and Templates: Rigid, template-based EHRs force excessive clicking and drop-down navigation, which slows charting and compromises medical quality.
- Data Siloing: Patient records, lab results, and claims often sit in isolation across different systems, making accountability and care coordination difficult.
- Inaccurate Provider Data: Outdated provider directories hinder operational efficiency and risk non-compliance, leading to significant revenue loss from claim denials.
- The "Governance Lag": 56% of medical groups lack formal policies on AI use, leading to "Shadow AI," where staff use unapproved consumer tools that risk leaking sensitive patient data.
- Interoperability Barriers: Only 8% of primary care physicians find it "very easy" to use information from different EHR developers.
3. Modern Data Management Solutions
To overcome these pain points and the systemic "governance lag" and fragmented data silos that currently buckle the system, physician-owned practices must transition toward clinical-first technologies that prioritize relationship-driven care over administrative rote. The emergence of "agentic AI" systems capable of executing multi-step workflows like identifying care gaps and handling intake marks a turning point for independent practices.
High-Impact Solutions:
- AI-Driven, Template-Free EHRs: Next-generation systems like Praxis EMR use "Concept Processing" to learn a physician’s unique style, allowing for free-text documentation that gets faster as it is used.
- Ambient Clinical Documentation: Tools like Nuance DAX Copilot and Suki use natural language processing (NLP) to listen to patient visits and generate visit notes automatically, reducing note-taking time by up to 72%.
- Provider Data Management (PDM): Centralized directories like Atlas PRIME use AI to validate provider information at the primary source, ensuring 95% accuracy and streamlining credentialing.
- Telehealth and Remote Patient Monitoring: 71.4% of physicians now use telehealth, though use is slightly lower in private practice (68.4%) compared to hospital settings (79.7%) due to implementation costs.
Even more important, adopting modern data management, analytics and AI/ML baked solution lies in a strategic shift from legacy business intelligence to Decision Intelligence, a unified approach that integrates data preparation, business analytics, and data science into a single frictionless environment.
The Pyramid Analytics Decision Intelligence Platform directly addresses critical management pain points by providing multi-source direct access to "dark" or "trapped" clinical data across disparate EMR and financial systems without the need for costly, time-consuming data duplication. Utilizing its high-speed "PYRANA" direct query engine, the platform delivers 10x faster performance than traditional tools, allowing practices to uncover the root causes of financial leakage or care gaps in real-time.
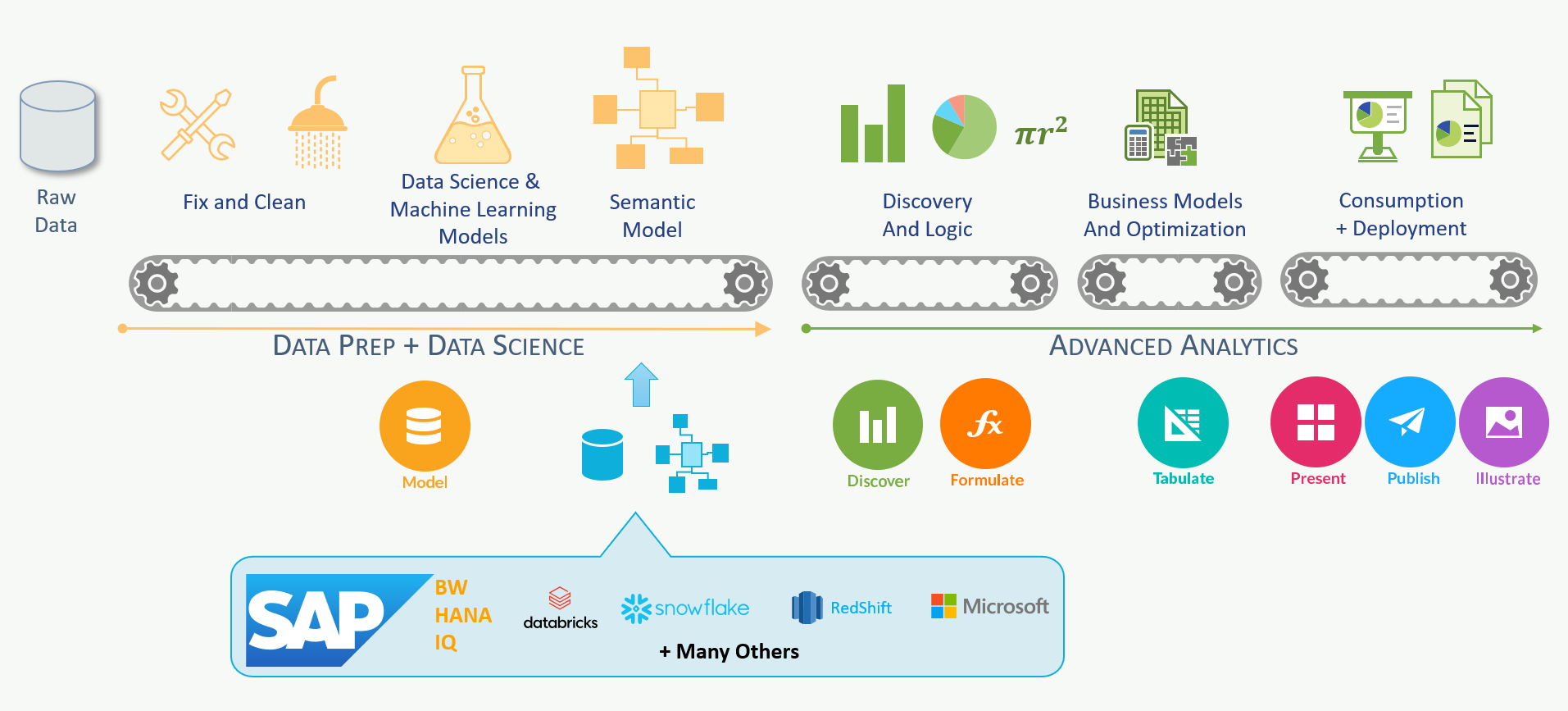
Furthermore, Pyramid’s AI-automated "Smart Insights" and Generative BI capabilities empower non-technical staff to interact with data conversationally, effectively lowering the skills barrier for sophisticated analytics. By democratizing data from the C-suite to the frontline, practices can achieve significant ROI as evidenced by The Physician Alliance, which saved $350,000 annually and future-proofed their operations through Pyramid’s virtual semantic layer and governed self-service.
Improve Operations with Data Analytics and Reporting
Effective reporting transforms data from a burden into a tool for operational success. Most health systems still lack a sophisticated understanding of the root causes of their financial losses. Transitioning to a data-driven management style requires metric-driven dashboards that inform both clinical and strategic decisions.
Recommended Dashboard Metrics for Private Practice:
- wRVUs (Work Relative Value Units): A core indicator of provider productivity.
- Collections: Real-time visibility to avoid cash flow surprises.
- Denial Rates: Identifying transposed numbers or credentialing issues that disrupt revenue.
- Compensation vs. Production: Evaluating fair market value and risk related to provider retention.
Case Study: The Physician Alliance - By bringing analytics in-house using the Pyramid Decision Intelligence Platform, this organization saved $350,000 annually. They democratized "trapped data," allowing physicians to use AI-automated "Smart Insights" to manage patient fees and costs more effectively.
Navigating AI Governance and Ethical Considerations
As AI becomes the system, the risk of "AI hallucinations" (confabulations) and algorithmic bias must be addressed through a "human-in-the-loop" framework. Governance is not just about compliance; it is the cornerstone of trust in the healthcare ecosystem.
The FAVES Principles for Responsible AI:
- Fair: Does the AI behave differently across patient populations?
- Appropriate: Is the use case suited for AI or does it require end-to-end human judgment?
- Valid/Effective: Is there evidence the tool works in a specific specialty mix?
- Safe: What is the failure mode, and how will it be caught?
Data Quality Pillars:
Practices should adopt an Information Quality Framework based on:
- Objectivity: Ensuring accuracy and completeness.
- Utility: Focusing on relevance and interpretability.
- Integrity: Protecting data through encryption and access controls.
- Standardization: Ensuring data follows established formats to eliminate confusion.
4. The 2026 Strategic Roadmap for Practices
To navigate the $1 trillion transformation toward digital-first care, CEOs must pivot from legacy "non-believer" models to a data-intelligent operating chassis. This roadmap leverages Decision Intelligence to bridge the gap between administrative rot and clinical excellence. By adopting the Pyramid Analytics Decision Intelligence Platform, practices can unify data preparation, business analytics, and data science into a single, frictionless environment. Successful translation of technology into practice requires intentional change management. Leaders must prioritize infrastructure that is "virtual by design" and "data-intelligent".
Actionable Steps for CEOs:
- Scale Governed Adoption: Deploy AI-driven, self-service experiences that empower non-technical staff with "Smart Insights," drastically reducing IT backlogs.
- Audit Current AI Use: Identify "shadow AI" and provide safe, approved paths for staff.
- Standardize Workflows: Create a standard operating chassis so that all nursing and administrative units use the same tools.
- Break Silos - Fully Leverage your Data": Use multi-source direct access to query trapped clinical and financial data in real-time without costly duplication.
- Prioritize Cognitive Productivity: Automate repetitive cognitive tasks to restore clinician capacity for high-value patient relationships.
- Invest in Upskilling: 75% of data leaders say employees need upskilling in data literacy to use AI responsibly.
- Anchor Strategy in Relationships: Measure AI success by its capacity to restore face-time with patients.
5. Conclusion
The year 2026 represents a definitive inflection point for physician-owned private practices, as the U.S. healthcare system transitions from a 5 trillion infrastructure−heavy model toward a proactive, digital−first ecosystem. Driven by an aging population that will soon see more Americans over 65 than under 18, the industry is witnessing a 1 trillion reallocation of annual spending toward personalized medicine and AI-supported decision-making. For the independent clinician, long-term sustainability requires navigating a complex "trust paradox" by moving beyond the role of administrator currently losing over 1.5 days a week to paperwork to becoming a data-orchestrator who prioritizes high-value clinical judgment over administrative rote.
The Pyramid Analytics Decision Intelligence Platform serves as the critical operating chassis for this transformation, providing multi-source direct access to siloed information to eliminate the "dark data" bottlenecks that traditionally stifle care coordination. By adopting unified platforms that integrate data science, preparation, and business analytics into one frictionless environment, practices can shift from episodic, reactive treatments to continuous, predictive care models. Ultimately, the strategic implementation of robust AI governance and template-free technological solutions will enable physicians to recapture their "pajama time," reinforcing the human patient-physician relationship as the primary driver of value in a data-intelligent market.
6. References
American Medical Association. (2025, December 29). Practice ownership linked to physicians’ use of telehealth. This report provides comparative data on telehealth adoption between private and hospital-owned practices, highlighting that 68.4% of private practitioners utilize telehealth versus 79.7% in hospital settings.
Atlas Systems. (2026, January 4). Best Provider Data Management Software. This source details PDM solutions like Atlas PRIME, which achieves 95% data accuracy through direct primary source validation.
Crossette-Thambiah, G., Berleant, D., & AbuHalimeh, A. (2024, September 26). An Information Quality Framework for Managed Health Care. Published in the Journal of Healthcare Leadership, this study establishes the foundational pillars of objectivity, utility, integrity, and standardization for clinical data management.
Elation Health. (2026, January 20). Predictions for Primary Care in 2026. Insights from primary care leaders regarding the shift from administrative efficiency to predictive care and the integration of AI-native operational tools.
Everson, J., Hendrix, N., Phillips, R. L., et al. (2024, March 26). Primary Care Physicians’ Satisfaction With Interoperable Health Information Technology. JAMA Network Open. This original investigation reveals that only 8% of primary care physicians find it "very easy" to use data across different EHR systems.
Harrop, C. (2026, January 21). AI governance in medical group practices: Rules for the humans in the loop. MGMA Stat. This resource outlines the FAVES principles (Fair, Appropriate, Valid, Effective, Safe) for responsible AI implementation and addresses the "governance lag" in medical groups.
Informatica. (2026, January 27). New Global CDO Report Reveals Data Governance and AI Literacy as Key Accelerators in AI Adoption. This study identifies the "trust paradox", where high internal trust in data exists despite a 76% lag in formal organizational governance.
IntuitionLabs. (2026, January 19). Impact of Artificial Intelligence on Clinical Data Management in the United States. Laurent provides data on ambient documentation tools, noting that AI assistants can reduce clinical note-taking time by 72% and eliminate "pajama time" charting.
Praxis EMR. (2026, February). Physicians choose their top 10 EHR systems for 2026. This update evaluates template-free EHR solutions and their impact on reducing professional stress and administrative rote.
PwC. (2025, September 17). From breaking point to breakthrough: the $1 trillion opportunity to reinvent healthcare. This vision document identifies the shift toward data-orchestration and the fact that physicians currently lose more than 1.5 days a week to paperwork.
Pyramid Analytics. (n.d.). The Physician Alliance Case Study: Future-proofing its business. This case study documents how a physician-led organization saved $350,000 annually and democratized "trapped data" using a unified decision intelligence platform.
Robeznieks, A. (2025, May 27). Ready for health AI? It may depend on your practice setting. American Medical Association News Wire. This analysis highlights the AI use gap, showing 72% adoption in hospital-owned practices compared to 64% in private practices.
Society of General Internal Medicine. (2025, February). Recommendations for Clinicians, Technologists, and Healthcare Organizations on the Use of Generative Artificial Intelligence in Medicine. A position statement outlining the ethical and clinical requirements for human-in-the-loop AI systems.
 Request a meeting
Request a meeting
 Email
Email Call
Call EN
EN
 FR
FR
 ES
ES


















Add Comments